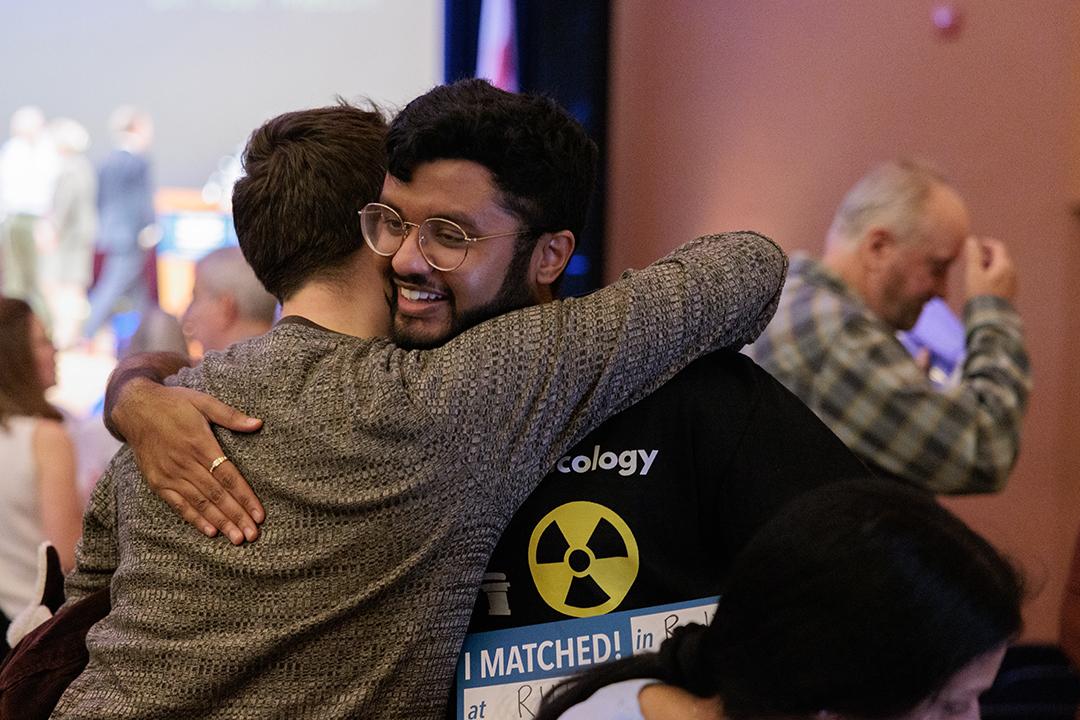
Lisner Auditorium hummed with anticipation leading up to noon on March 15, as the George Washington University School of Medicine and Health Sciences (SMHS) M.D. Class of 2024 received their envelopes from the National Residency Matching Program (NRMP), eager to discover where they will continue their training as physicians.
It was a traditional culmination for a class that began its medical education under very different circumstances. They were the COVID class, students who began medical school socially distanced, with much of the fanfare celebrating their arrival delayed nearly two years until the city’s pandemic restrictions eased.
“This class is special for several reasons,” said Barbara L. Bass, dean of SMHS. Recalling her first match day as dean of the school four years ago just as the COVID-19 pandemic had been declared, Bass, who also serves as professor of surgery, Bloedorn Professor of Administrative Medicine, vice president for health affairs and CEO of the GW Medical Faculty Associates, noted that the Class of 2024 began their medical education virtually, due to the tight COVID restrictions.
“You all … have been a remarkably resilient group that has learned so much during this time,” she said, welcoming the students as well as the family, friends and faculty on hand to cheer them on. “You have demonstrated your commitment, determination and your support for one another.”
The Class of 2024 is also special for another reason, matching during the school’s year-long Bicentennial Celebration. Bass noted that establishing a medical school was part of GW’s original charter signed by President James Monroe and approved through an act of Congress in 1821.
“A core element of that charter was a commitment to medicine, to education, to training the next generation [of physicians], to doing all those things that you are doing with us today,” said Bass. “Today, you get to see [where] the next focus of that training will come from.”
Celebrating the ‘joy and privilege of medicine’
In honor of dual milestones for the school and students, Bass invited Kevin O’Connor, the 16th physician to the president of the United States and associate professor of health, human function and rehabilitation sciences at SMHS, to deliver a special keynote address, “The Joy and Privilege of Medicine.”
In his remarks, O’Connor set out to show how he sees the practice of medicine as “an absolute privilege,” as well as exploring the concept of joy, how physicians may be a source of joy for their patients, and how young doctors can ensure they live their lives, not just their practice, with joy.
To prepare, he turned to SMHS’ Himmelfarb Library but was disappointed to discover most of the available literature wasn’t about the joy of medicine as much as it was about combating physician burnout.
“At least for me,” he said, “the absence of burnout is not joy. Our aspirations should not simply be to put off burnout for as many years as we can. Our aspirations should be to thrive.”
He touched on the importance of being present and noticing and accepting life’s little joys and the value of offering a simple assurance of recognition.
O’Connor described a Zulu greeting he picked up on his travels, that best expressed the idea — sawubona, or “I see the whole of you.”
“The notion that someone sees you is really important to us as human beings,” he said. “It’s important for us to convey to and for our patients for their healing. And it’s equally important for us as individuals for our resilience and our capacity to accept joy.”
The salutation, O’Connor said, “recognizes the worth and the dignity of the person being greeted.”
The traditional response, he continued, was shiboka, or “I exist for you.”
“These aren’t simply greetings, they are ways to revitalize and affirm the other person, giving full attention and presence, communicating that you see and cherish them as a person,” O’Connor explained. “Doesn’t that sound like something we should probably aspire to weave into our practices?”
Match migration
The annual event marks the pinnacle of four years of medical school, following years of classroom cramming, clinical rotations and a year-long quest to find the ideal program to complete one’s medical training in a chosen medical specialty.
The nationwide process was created by NRMP in 1952, based on a Nobel Prize-winning algorithm that blends medical student preferences with those of residency programs to ensure each gets as close to their top choices as possible.
From Maine Medical Center in Portland and Brigham and Women’s Hospital in Boston to University of Miami Jackson Health System in Miami GW’s MD Class of 2024 dominated the I-95 corridor, with more than half of the class landing an East Coast residency. In all, students fanned out across 34 states and the District of Columbia, with Patrick Shaw planting a GW Revolutionaries flag at Tripler Army Medical Center, outside Honolulu marking the school’s furthest westward expansion.
While specialties such as internal medicine, pediatrics, anesthesiology, psychiatry and emergency medicine were the overwhelming leaders in this year’s match, programs including otolaryngology, interventional radiology and vascular surgery were also represented.
Finding that special specialty
Alexandra Tunkel was among five members of the class to match in otolaryngology, or the ear, nose, and throat (ENT) specialty.
“I could spell it at three years old,” she joked, as she described her match.
Tunkel will take that next step in her medical career in a familiar specialty at a familiar place, Johns Hopkins University. Her parents David Tunkel and Theda Kontis, both otolaryngologists, met at the Baltimore university during residency roughly 30 years ago.
“I definitely made my list location based, I wanted to be in the Mid-Atlantic region,” she said, adding, “I also really valued my time with the residents [at Hopkins]. I was able to have an in-person interview, and I was really able to see myself there.”
Although both otolaryngology and Johns Hopkins were fixtures throughout her childhood, neither was a given as she entered medical school. The blend of clinical time, surgical time and long-term patient care, however, made ENT appealing. “Very few surgical specialties afford that kind of long-term follow-up care. So that’s what led me to ENT.”
That and great mentors, at home and in school.
For classmates Hari Magge and his partner Porshad Elie, narrowing their choices was a little more complicated. The two opted to enter the couples match, a common process for those who are married or in a relationship, where students rank their preferences as pairs.
“We did a couples match so we could be sure to end up in the same city,” Magge said. “You rank every single permutation from top to bottom. Statistically, we have the same odds as matching, regardless of whether or not you do a couples match. But we did this so we could try and be in the same place.”
For Magge and Elie, it involved sitting down for long discussions about the best mix of programs and locations. Ultimately, the results couldn’t have been scripted better if they were written in Hollywood. Hagge matched in otolaryngology at Cedars-Sinai Medical Center in Los Angeles, where he had done a month-long rotation. And Elie? She matched in pediatrics in her hometown, at Kaiser Permanente, Los Angeles, a short drive away by LA standards.
Rushi Challa managed to thread the needle between his chosen specialty and staying close to home. With his parents in Virginia, Challa weighed location heavily, but a competitive specialty made closing the gap between program and proximity a bit tougher. There is just one area institution offering a vascular surgery residency —MedStar Washington Hospital Center — but Calla’s impressive clinical and research background helped close the deal.
It was during his third year that he “discovered surgery.” On his rotations he had an opportunity to explore vascular surgery. “I just enjoyed the finessing and the beauty. Since then I was hooked.”
“The field is incredibly innovative,” he added. “There are so many new advances coming, in terms of use of technology and device development, and I want to be part of that trend. Working on new devices is something I am very passionate about.”
Challa found a mentor at GW in Bao-Ngoc Nguyen, associate professor of surgery, who included him on some research projects. “That’s where I started my vascular journey and got the itch to continue,” said Challa.
More matches
The GW SMHS International Medical Program (IMP) and the Office of Graduate Medical Education also had students to place and slots to fill on Match Day.
Two fourth-year medical students in the IMP MD Program for International Students applied and successfully matched in their respective specialties, emergency medicine and plastic surgery. Seven members of the International Sponsored Residency Program, matched in specialties including internal medicine, pediatrics and neurology. Five members of the Medical Research Fellowship Program also successfully matched in U.S.-based residency programs.
The Office of Graduate Medical Education filled all of its 116 available positions across 16 programs.
Students from 52 U.S. medical schools, including nine osteopathic programs and 14 international institutions, will be joining GW’s academic medical enterprise this June. Among the new trainees, 19 GW students matched here at home, and 11 others come to Foggy Bottom from regional medical schools — Howard University, Georgetown University, University of Maryland, University of Virginia and Virginia Tech.
See where GW’s Class of 2024 matched and watch the video of the event.