By Kristen Mitchell
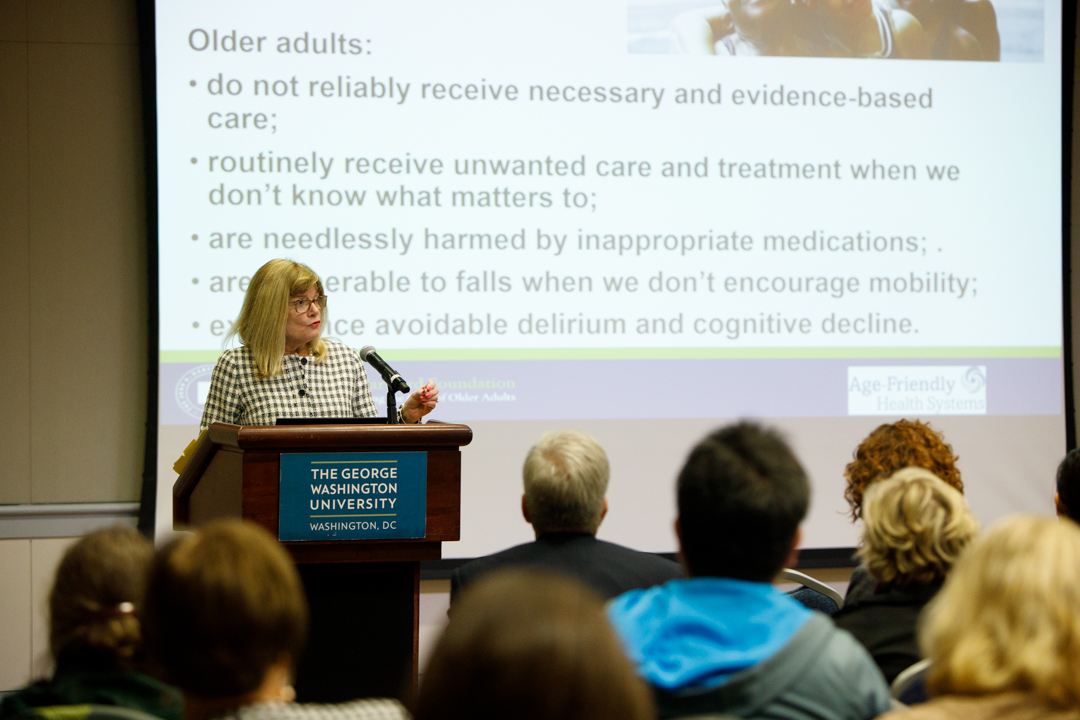
Building a health care system oriented for the needs of aging adults should be a priority for health care professionals, according to Terry Fulmer, a registered nurse and president and chief strategist for the John A. Hartford Foundation, a New York-based foundation dedicated to improving health care for older adults.
Eighty-percent of Americans 65 and older have a chronic illness, and 77 percent of them have at least two. These individuals frequently engage with a health care system that causes harm and overlooks their specific needs, she said.
“Each of you can see yourself in this work. Any of us are only one click away from a person...who’s had a negative experience in the health care setting because it wasn’t age friendly,” Dr. Fulmer said. “They had a medication problem, they fell, they were not respected in their choices around the care they needed…. We want to eradicate that.”
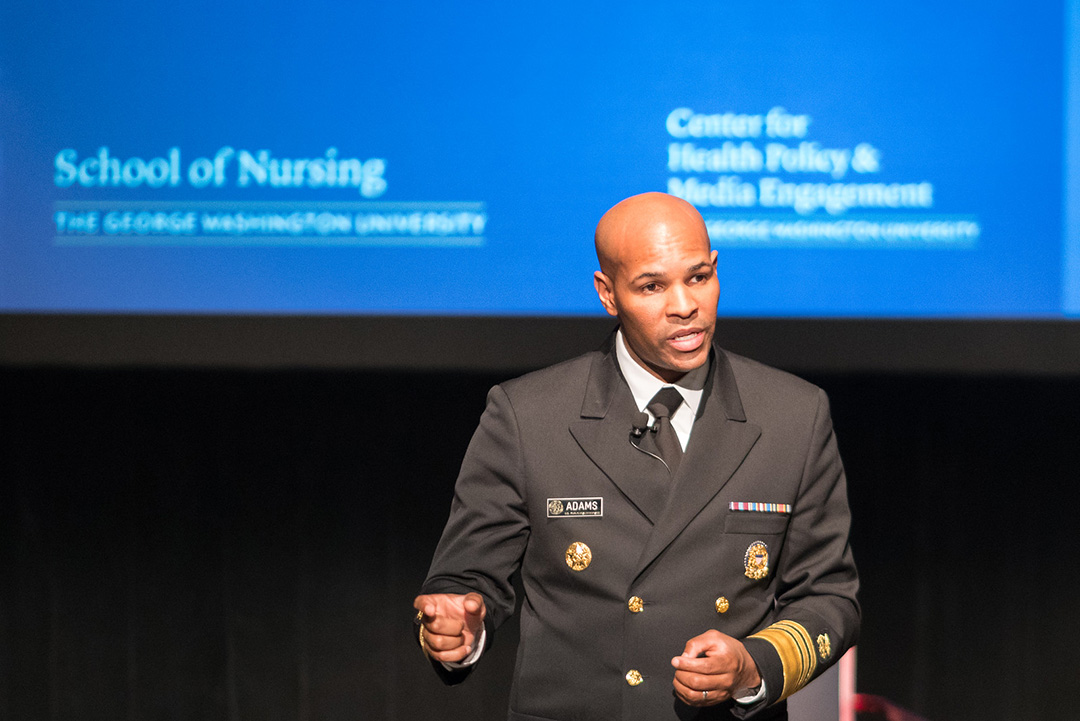
Dr. Fulmer spoke in the Marvin Center Continental Ballroom on Tuesday as part of the Health Policy Leadership Lecture Series event. The series is co-sponsored by the George Washington University School of Nursing’s Center for Health Policy and Media Engagement and Center for Aging, Health and Humanities.
Melissa Batchelor-Murphy, associate professor of nursing and geriatric nursing researcher, said health professionals need to urgently focus on improving age-friendly health systems. In the next 11 years, all baby boomers will have reached age 65. For the first time in U.S. history, the country will be home to more older adults than children, she said.
The goal is to create health systems that prevent harm to older adults, improve health outcomes and lower overall costs by “adopting evidence-based models and practices to deliver better care to our rapidly aging population across care settings,” Dr. Batchelor-Murphy said.
The push for age-friendly health systems is a social movement, Dr. Fulmer said. Health care professionals should focus on what matters most to the patient when prescribing care, including end of life care. They should use age-friendly medications that do not interfere with issues such as mobility and help them achieve their care goals. Care should also focus on preventing, identifying, treating and managing conditions like dementia, depression and delirium.
It’s important that care providers ensure older adults move safely every day to maintain function and to help them continue living a fulfilling life, she said. One key aspect of creating sustainable change in this area is incorporating reliable, evidence-based models that have proven effective. It can take nearly 15 years for best practices to be fully incorporated in the health care system, and care providers should focus on closing this gap.
“We want to make sure that every older person gets reliable care that improves their health care outcomes and meets their goals of care,” Dr. Fulmer said.
Right now, this type of evidence-based geriatric care is only reaching about one in 10 patients that could potentially benefit. Better care and communication across the health system, from primary care doctors to emergency room care, will greatly improve the experience for individual patients. Complexity is fine, Dr. Fulmer said, confusion is not.
“We know we can do better,” she said. “We believe that our age-friendly health system work is one way to try to make that work better.”