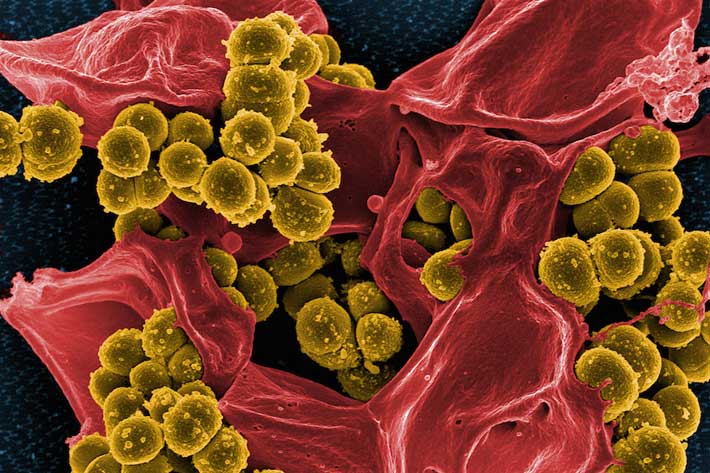
Staphylococcus aureus, better known as staph, resides in the nose, often unbeknown to its human host.
Generally, these bacteria go unnoticed or cause problems no greater than minor skin infections. But if staph invades deeper into the body, an infection can turn deadly. Worse yet, some strains of the bacteria no longer respond to antibiotics. A drug-resistant form of staph, called MRSA—Methicillin-Resistant Staphylococcus aureus—kills more than 11,000 people in the United States each year, according to the Centers for Disease Control and Prevention.
“Staph is an asymptomatic colonizer. It can live on us and spread silently to other people without ever showing any signs,” said Lance Price, a professor at the George Washington University. “But once there is an opportunity—if you get sick or have a break in your skin— these bacteria can infect you.”
Dr. Price and Cindy Liu, both faculty members in the Milken Institute School of Public Health, believe they have identified an unlikely weapon against these infections. Their study, published in the AAAS journal Science Advances this summer, suggests that certain types of “good” bacteria in the nose have the ability to eject staph from its home.
“Historically in medicine, all bacteria are ‘bad.’ With my training in ecology, I am of the mindset that there are both good and bad bacteria, that the story is more complex,” said Dr. Liu, a medical doctor. “By understanding this complex story, we might be able to come up with new ways to prevent or to treat infections.”
The nasal microbiome is a collection of the many different microbes that take residence within the nose. The GW researchers were curious to find out about the variation in the amount of staph present there: Why do some people have an abundance of the bacteria while others have hardly any? Most experts have assumed that genetics played a role.
To test the theory, the research team looked at data taken from 46 pairs of identical twins and 43 pairs of fraternal twins in the Danish Twin Registry, which comprises information about almost all twins born in Denmark since 1870. Using new molecular tools developed in Dr. Liu’s lab, the researchers were able to analyze the various DNA samples to uncover not only what types of bacteria were present but also the amount of each kind.
Surprisingly, the researchers discovered no correlation between twin pairs and their nasal microbiome, showing that a person’s risk of carrying staph is not genetically predetermined.
“So, the next thought was maybe there is something other than our genes that could be modifying our ability to become colonized with staph,” Dr. Price said. “And we already know that there can be these antagonistic relationships between bacteria. Some bacteria play well together while others don’t.”
Indeed, the researchers found that some types of bacteria don’t make good neighbors with staph. They saw that often when a non-pathogenic bacteria called Dolosigranulum was present, staph was not, and it appears to be a dose-dependent relationship. People who have Dolosigranulum are less likely to carry staph, and the more Dolosigranulum you have, the lower the abundance of staph.
This was good news for the researchers, who think they may be able to use a probiotic approach to introduce the good bacteria into the nose and boot out staph.
“It’s exciting because most people who are talking about probiotics are thinking about yogurt and our gut, and sometimes vaginal health,” Dr. Price said, “but now we’re talking about probiotics that you could put in your nose.”
Another key finding in the study is that although men tended to have more staph bacteria in their noses, both sexes were equally as likely—around 50 percent—to be colonized. This conclusion dispels a long-held acceptance that the bacteria are likelier to colonize men. These results were so unexpected, in fact, that the researchers had to go back and check their data multiple times.
“In the end, I think what we found made sense. Nobody has looked at the nasal microbiome using our method,” Dr. Liu said. “You can explain the differences between sexes from the earlier studies, because the method they used was really sensitive to how much bacteria was present. Because men tend to have higher counts, their bacteria were just more likely to be detected.”
The discovery could have implications for screening patients who are at high risk of contracting a staph or MRSA infection, like young children or those who work in hospitals, the researchers say. The current culturing method that doctors use to test for these infections may not detect the small amounts of the bacteria in people carrying low abundance of staph, which can be problematic.
“The less bacteria you have, the less likely you’re going to come up positive on culture,” Dr. Price said. “Our findings show that those who carry low amounts of staph, which are often women, could be unknown reservoirs of staph and spread it to others who can carry more.”
The revelation could potentially move screening methods away from culturing tests and in the direction of molecular testing, he added.
The next steps for the researchers will be to recreate their own bacterial “turf wars” in a petri dish to see how well the good bacteria can eliminate staph.
“We’re going to create a model human nose and introduce bacteria,” Dr. Price said. “Then we’ll have little fights to pit staph against Dolosigranulum, let them duke it out and see what happens.”